Challenging the HbA1c? When 7% becomes irrelevant (by CDE Kate Mundy)
The almighty HbA1c! It’s the test all people with diabetes undertake several times a year. It is the test most often quoted on forums, in GP and specialists offices and in every day diabetes life. It is arguably the most anticipated and anxiety provoking test for people living with diabetes. But what is it really? How relevant is it in the context of our everyday diabetes management?
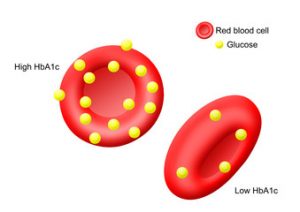 Put simply, a HbA1c measures how many of our red blood cells are saturated in sugar and comes up with a number which indicates how “well controlled” blood glucose has been over the past 90 days. People without diabetes will have a HbA1c of around 4-6%. In diabetes, the aim is to have a HbA1c of 7% or less (or an average blood glucose of about 8).
Put simply, a HbA1c measures how many of our red blood cells are saturated in sugar and comes up with a number which indicates how “well controlled” blood glucose has been over the past 90 days. People without diabetes will have a HbA1c of around 4-6%. In diabetes, the aim is to have a HbA1c of 7% or less (or an average blood glucose of about 8).
There is excellent evidence that supports a HbA1c of 7% or less significantly reduces the risk of long term complications in those with Type 1 and Type 2 diabetes.
BUT there are significant flaws in relying solely on HbA1c to measure diabetes success.
A HbA1c is an average. That works for the person whose diabetes does not fluctuate drastically and has stability. However, in people whose diabetes behaves like a moody teenager with rapid and unpredictable variation, the HbA1c does not account for high and low blood glucose levels throughout the entire day. In this context, a person can have a HbA1c of 7% or less and be experiencing extreme and dangerous episodes of hypo and hyperglycaemia. It can be argued that the medical profession, by placing so much emphasis on HbA1c, can easily overlook this feature.
Does a Hba1c measure stability? Does it measure the patient effort in managing their diabetes on a day to day basis? Does it measure quality of life? No! Then why do we as a community rely so heavily on it? Do these things not matter as long as we have a good HbA1c?
As a diabetes community, HbA1c has almost become a competition where those who reach target are hailed by their doctors as having “excellent control”; congratulated by their peers on “ a job well done” and denotes a feeling of achievement. But does this equal success in diabetes management?
A HbA1c is a number. It’s a tool. But it is really not worth much in someone with rapidly fluctuating BGL’s. Is it time we started to measure success in diabetes management in different ways? Or at the very least, stop relying so heavily on a measurement that, in the world of diabetes becomes irrelevant without looking at the “bigger” picture.

This also brings up another query. Ive noticed if i have to fast before a bloodtest eg. getting my kidney test & hba1c at same time my overall average is always lower than if im not having to fast. my hba1c will be a tad higher if i dont have to fast/ if ive eaten beforehand. ive only noticed this in the last few years i do believe what blood sugar you are at the time does make a difference. Has anyone else noticed this?
Hi Fiona,
It is interesting to note that there are many things that influence HbA1c. HbA1c appears to be more impacted by the past months blood glucose control that than the previous 2 months. Iron levels, haematocrit, B12 also influence the accuracy of HbA1c as well as some medications. Whilst I am not sure whereas a fasting vs a non fasting state is noted to impact, I do believe everybody is individual. I have attached a link to a journal article you may find interesting.
http://journals.aace.com/doi/pdf/10.4158/EP161209.CO